The Flesh-Eating Bacteria is a misunderstood, deadly and aggressive disease.
What is necrotizing fasciitis?
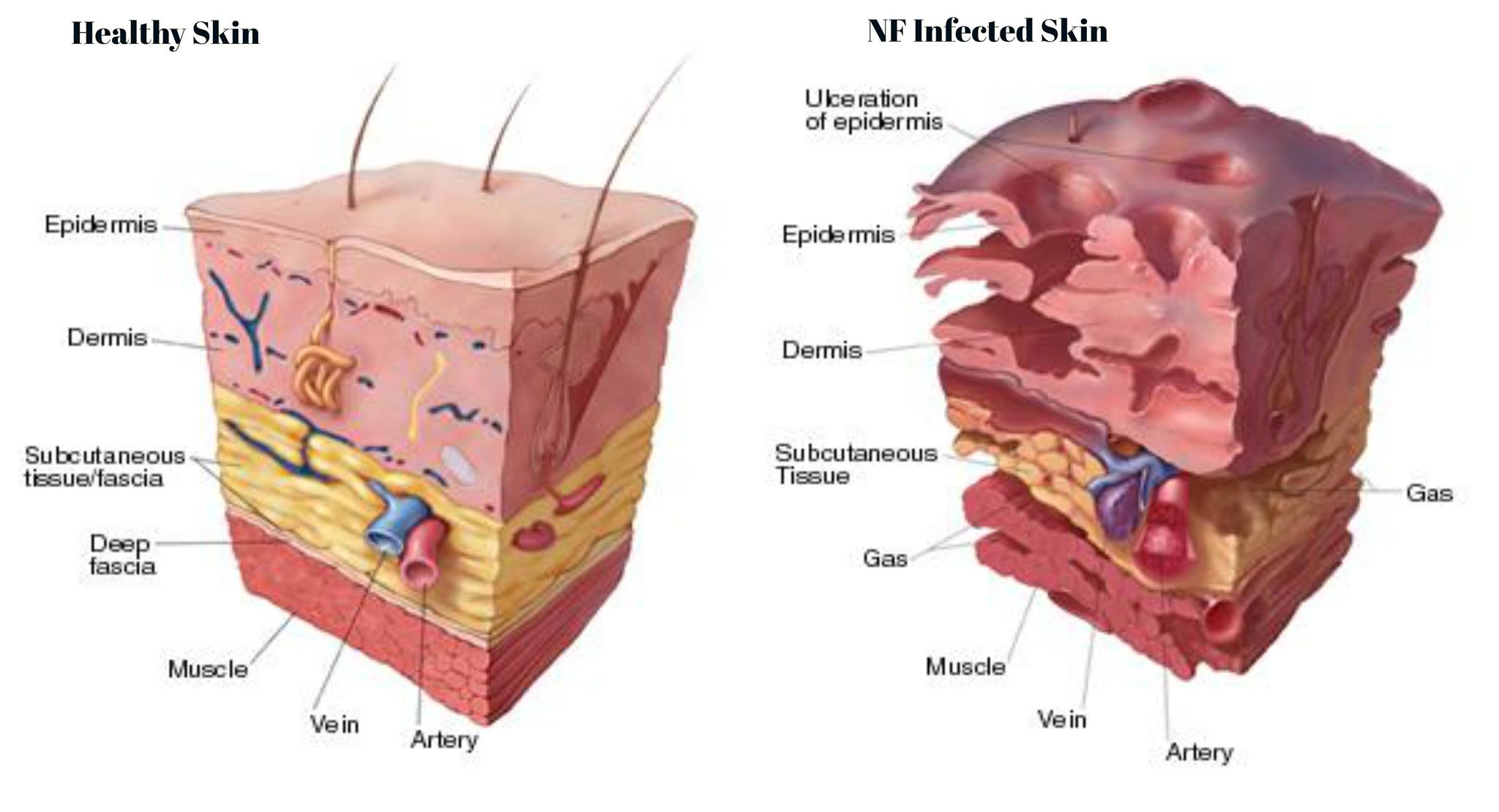
Necrotizing fasciitis is an infection caused by bacteria. In some cases, it is unknown how the infection began. Once it takes hold, the infection rapidly destroys muscle, skin, and fat tissue within a very short time. The disease is sometimes called flesh-eating bacteria. When it occurs on the genitals, it is called Fournier gangrene.
Necrotizing fasciitis is very rare but serious. About 1 out of 4 people who get this infection die from it. Many people who get necrotizing fasciitis are in good health before they get the infection.
Your risk of getting this infection is higher if you:
Have a weak immune system.
Have chronic health problems such as diabetes , cancer, or liver or kidney disease.
Have cuts in your skin, including surgical wounds.
Recently had chickenpox or other viral infections that cause a rash.
Use steroid medicines, which can lower the body's resistance to infection.
What causes necrotizing fasciitis?
Necrotizing fasciitis is caused by several kinds of bacteria. Some of these bacteria also cause infections such as strep throat and impetigo. Usually, the infections caused by these bacteria are mild. But in rare cases, they can cause a more dangerous infection.
You can get necrotizing fasciitis when bacteria enter a wound, such as from an insect bite, a burn, or a cut. You can also get it in:
Wounds that come in contact with ocean water, raw saltwater fish, or raw oysters, including injuries from handling sea animals such as crabs.
An intestinal surgery site, or in tumors or gunshot injuries in the intestines.
A muscle strain or bruise, even if there is no break in the skin.
The bacteria that cause necrotizing fasciitis can be passed from person to person through close contacts, such as touching the wound of the infected person. But this rarely happens unless the person who is exposed to the bacteria has an open wound, chickenpox, or an impaired immune system.
What are the symptoms?
The symptoms often start suddenly after an injury. You may need medical care right away if you have pain that gets better over 24 to 36 hours and then suddenly gets worse. The pain may be much worse than you would expect from the size of the wound or injury. You may also have:
Skin that is red, swollen, and hot to the touch.
A fever and chills.
Nausea and vomiting.
Diarrhea.
The infection may spread rapidly. It quickly can become life-threatening. You may go into shock and have damage to the skin, fat, and the tissue covering the muscles. (This damage is called gangrene .) Necrotizing fasciitis can lead to organ failure and death.
How is necrotizing fasciitis diagnosed?
The doctor will diagnose your infection based on how suddenly your symptoms started and how quickly the infection is spreading. The infected tissue may be tested for bacteria. You also may need X-rays, a CT scan, or an MRI to look for injury to your organs or to find out how much the infection has spread. The medical profession often refers to NF as NSTI (Necrotizing Soft Tissue Infection)
How is it treated?
Early treatment of necrotizing fasciitis is critical. The sooner treatment begins, the more likely you will recover from the infection and avoid serious complications, such as limb amputation or death. You may be treated in the intensive care unit (ICU) at the hospital.
Treatment may include:
Surgery that removes infected tissue and fluids to stop the spread of infection. Surgery is almost always needed. Most people need several surgeries to control the infection. Removing limbs (amputation) or organs may be done to save the person's life, depending on how severe the infection is and where it has spread.
Medicines (such as antibiotics ). These kill the bacteria causing the infection.
Procedures to treat complications such as shock, breathing problems, and organ failure.
Hyperbaric oxygen therapy.
Is it possible to prevent necrotizing fasciitis? Is necrotizing fasciitis contagious?
Necrotizing fasciitis does not begin unless an infection has already started in tissue; immediate effective treatment of any infection is likely to prevent the disease. Further, anything that can help prevent infections will help prevent necrotizing fasciitis. Practices such as hand washing, checking extremities for cuts or wounds if you have diabetes, avoiding physical contact with people who carry MRSA, and good hygiene practices help prevent initial infections that may lead to flesh-eating disease. Immunosuppressed patients should be very careful not to get infections, and people with liver disease should avoid eating seafood that may be contaminated with Vibrio vulnificus. People with liver disease should not have any infections or cuts in the skin exposed to warm seawater to avoid necrotizing fasciitis caused by Vibrio vulnificus.
Physicians, surgeons, and other caregivers play an important role in prevention. Cases of necrotizing fasciitis may occur when surgical sites become infected. Consequently, physicians need to use sterile techniques when doing surgery and adhere to hospital practices such as glove and gown coverage to help prevent infection spread in hospitalized patients. Careful surgical techniques in sites that can easily become contaminated are required. Some examples of such sites are bowel surgery, episiotomy (surgically enlarging the vaginal outlet), and debridement with the closure of traumatic wounds.
Necrotizing fasciitis is not usually contagious. However, it is possible for uninfected people to physically come into contact with some patients with the disease and become infected with an organism that may eventually cause necrotizing fasciitis. For example, a person could come in contact with a lesion containing MRSA organisms causing or contributing to the disease in another person and then become infected with MRSA. Transmission from one person to another usually requires direct contact with a patient or some item that can transfer organisms like MRSA to another person's skin; infection usually requires a skin break (cut or abrasion) for the organisms to establish an infection (cross-contamination of infected wounds).